Chair, AANS/CNS Communications and Public Relations Committee
Mount Kismo Medical Group
Columbia University Medical Center
Mt Kisco, New York
Aging Population
Medicine is facing a real crisis. In fact, this monumental challenge hasn’t even attracted much attention of the media. Some attention has been given to costs associated with this demographic. However, across the country, neurosurgeons are coping with the escalating problems associated with the aging spine. Consider the following critical statistics — in the year 2020.
- There will be at least 75 million Americans over the age of 65;
- 14 million will have osteoporosis;
- Nearly 30 million have low bone mass;
- Patients over the age of 65 consume one-half of all health care dollars (over $80 billion) and one-half of all hospital days;
- Osteoporosis alone costs more than $20 billion annually;
- The typical age of a patient having spine surgery increased by more than five years (48.8-54.2) in the decade 1998-2008 and continues to rise dramatically; and
- Those who reach the age of 65 are likely to live nearly 20 more years.
As life expectancy has increased, there is the concomitant expectation of being able to lead an active and vibrant life. Too often the aging spine has different ideas.
The Aging Spine
Is it just bad luck or do our spinal columns age badly? Why are our spines so vulnerable? Our spinal columns serve two incredibly important functions. The first is providing protection for our spinal cord and nerves. To do this our spinal column must be very strong (think about a knight’s plated armor). However, the second function of our spine is to provide the primary support for all of our mobile activity, including the need for flexibility (think of all the bending, twisting and reaching we do just to get dressed). In order to serve both of these crucial tasks everyday or our lives, the spine is made up of a series of bones that require precise synchrony and connectivity, much like a complex set of gears in a machine. Unfortunately, this also means there are many small parts (joints, ligaments, tendons and muscles) that can show the effects of wear and tear over time. Osteoporosis serves to significantly aggravate this entire process in many ways leading to a downward spiral for the individual.
Osteoporosis
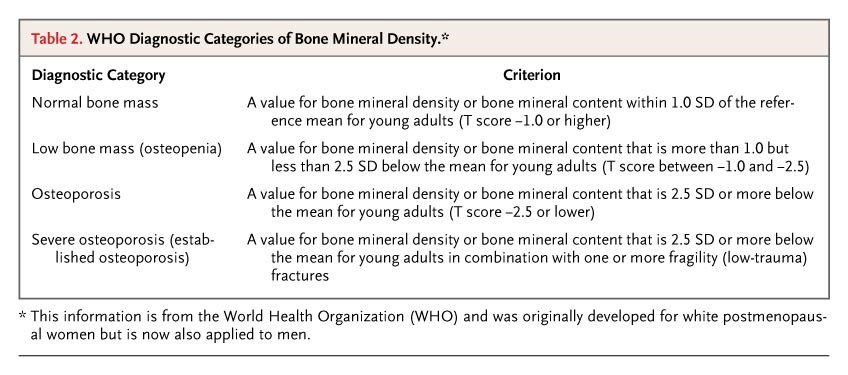
What is osteoporosis?
- A condition of skeletal fragility characterized by compromised bone strength predisposing to an increased risk of fracture.
Who gets osteoporosis?
- Everyone is at risk! While it is a disease of aging, it can strike at any age. Women have a much higher risk than men.
How is osteoporosis diagnosed?
- Screening should routine be performed using a simple test called a Bone Density Test (called a DXA scan).
Can osteoporosis be prevented?
- While osteoporosis may not be entirely preventable, there are definitely things that can reduce the risk of developing osteoporosis or sustaining the worst consequences (debilitating fractures) resulting from this disease.
Osteoporosis and Neurosurgery
Recently, a thin and active 92-year-old man came to my office with a primary complaint of having back pain that interfered with his three time a week tennis game. He was in remarkably good health, on no medication other than a baby aspirin, with no prior surgeries. Until recently, he had regularly walked several miles, played a vigorous game of tennis, and regularly attended a variety of cultural events in New York City. However, for the last six weeks, he experienced debilitating pain in his back and both legs whenever he played tennis more than 10 minutes or walked more than one block. His life, as he knew and loved it, had been thoroughly disrupted. Evaluating his spine revealed osteoporosis with marked degeneration resulting in a significant curvature (called scoliosis) and narrowing of the spinal canal (called stenosis) such that his nerves were being compressed. As a neurosurgeon, my challenge was to try and design an intervention that would help restore function and quality of life with limited risk.
Accepting the Challenge
Neurosurgeons across the country are addressing this new challenge in a variety of ways:
- We are carefully choosing patients who can benefit from surgical intervention to restore function and quality of life, even in the face of advancing age;
- We are working with our medical colleagues to identify at risk patients and get early intervention;
- We are providing professional and patient education programs;
- We are doing research to help better understand how to limit the risks associated with surgery when it is needed;
- We are using registries and other data to measure care delivery and outcomes in a meaningful way; and
- We are collaborating with our anesthesia colleagues in pre- and post-operative management of this higher risk population.
May is National Osteoporosis Month, the perfect opportunity to highlight the importance of our spines and the downward spiral that osteoporosis causes. The aging spine poses a real challenge for all of medicine right now, but neurosurgeons will continue to lead the way in finding solutions that help our patients live long and active lives.